Why COVID sleuths assume viral reservoirs 2023
Before the term “long COVID” was coined, Brent Palmer first suspected it.
His friends caught the virus while skiing and returned to Colorado with the mystery new ailment. Palmer, who researches HIV’s immunological response, found it terrifying and irresistible.
He wanted to know how their T cells, which fight infections, were managing the new infection. He took blood samples. One topic particularly attracted him. Six weeks after her acute sickness, she still had heart palpitations, chest aches, and problems breathing.
Palmer found in the lab that she had a much higher percentage of T cells aimed at the virus than her husband, who had also been unwell but had recovered. “They had very different responses,” says Palmer, a University of Colorado assistant professor of medicine.
As he studied more patients with these persistent symptoms, Palmer noticed that T cells aimed at the virus didn’t drop off after acute infection.
“These individuals had frequencies that were 100-fold higher in some cases than those that didn’t have any persistent symptoms,” he says.
Palmer said their body was still fighting the infection. “Despite testing negative in a nasal swab, is the virus still persisting in the lungs?” Is it in another organ?”
For years, scientists investigating long COVID have raised the same question. “Viral persistence” suggests that viral reservoirs in the body may cause long-term COVID symptoms in some patients.
As more evidence suggests that some people may have “viral reservoirs” after their initial illness, this line of research has gained momentum. It’s not the only theory, but some scientists think it’s the best.
“There’s enough evidence to place viral reservoirs as one of the leading drivers of long COVID,” says scientist Amy Proal, president of PolyBio Research Foundation, which is researching viral persistence.
A reservoir—where?
Evidence of the virus remaining in multiple places of the body and signals that the immune system is still revved up months after the acute illness have fueled viral persistence studies.
Palmer and his team found that long-term COVID patients had more virus-specific T cells, higher systemic inflammation, worse lung function, and longer-lasting symptoms like cough and difficulty breathing. Other teams have observed similar immune responses in long-term COVID patients.
Scientists have found virus genetic material or proteins in several body parts. Many months after infection, patients with persistent symptoms have virus in their stool and gut tissue samples. In other instances, biopsies from other sections of the body have shown that some individuals can recover virus pieces months later.
Last year’s meticulous autopsy study supported viral persistence.
Dr. Daniel Chertow found “virus in over 30 different cell types” and “in tissues throughout the body and all the major organs” in COVID-19 patients who died.
A person who died over 200 days after COVID-19 had virus genetic material. In another, Chertow and his team cultured virus from brain tissue samples from a patient who died within two weeks.
“It provides definitive evidence that the virus is capable of spreading all over the body and that it’s capable of persisting in parts all over the body,” says Chertow, an investigator at the NIH Clinical Center and the National Institute of Allergy and Infectious Diseases.
Since the study didn’t focus on long-term COVID patients, Chertow warns against extrapolating too much. The individuals were older and had health issues, unlike those with protracted COVID-19 who were healthy and had a mild case before developing chronic symptoms.
“Ultimately, the role of viral persistence in causing or contributing to clinical symptoms and signs that people with long COVID experience is yet to be determined,” he says, “but our paper provides strong biologic plausibility that it may contribute.”
Unanswered queries
Dr. Michael Peluso, a long COVID researcher at the University of California, San Francisco, believes this research has raised awareness of viral persistence following acute illness.
After researchers discovered that Ebola survivors could harbor viral reservoirs in parts of the body the immune system couldn’t reach, this was a “game changer” in our understanding of the disease. Peluso notes that extended COVID research has significant holes. People with persistent symptoms and those without have shown viral persistence.
“It does seem we can recover particles of this virus for much longer than we initially expected in at least some people,” Peluso says. “It’s not clear yet whether there is a direct relationship between these measurements and the person’s clinical condition.”
Mohamed Abdel-Mohsen, an associate professor at the Wistar Institute’s Vaccine and Immunotherapy Center, says there is “overwhelming evidence” of a viral reservoir in some people, but the “degree that contributes to the mechanism or the symptoms of long COVID” is unknown.
Multiple causes. What’s the connection?
However, researchers don’t expect viral persistence to explain all cases.
“No one thinks that every long COVID patient has the exact same thing happening,” adds Proal.
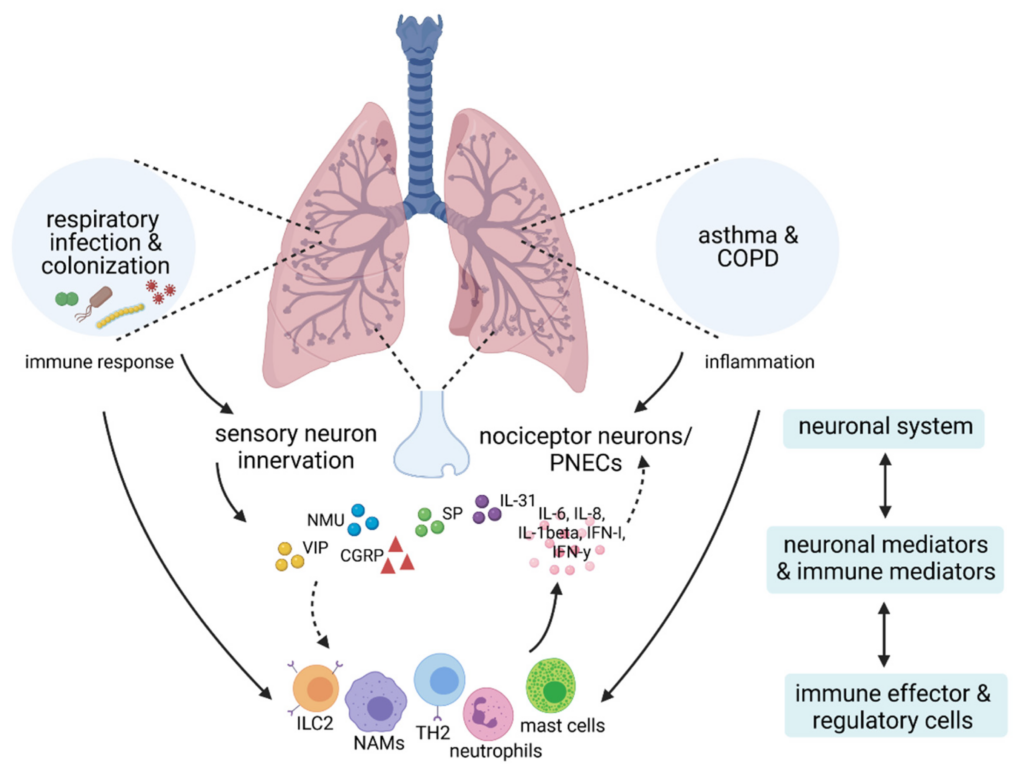
Other mechanisms are being considered. Autoimmunity and other immune system issues, micro blood clots and vessel lining inflammation, tissue damage, virus reactivation, and brainstem and vagus nerve signaling issues are among them.
“Right now, we have these buckets,” Peluso explains. “Ultimately, we need to connect all the dots and see how these different mechanisms might be interrelated and whether particular pathways relate to specific subsets of symptoms,” he says.
Long COVID definitions vary from research to study. While researchers have identified clusters of symptoms, the diagnosis can still be a catch-all for many post-COVID-19 issues, making it harder to study.
“Viral reservoir” can hide a mystery. What persists?
Peluso said long-term COVID patients don’t have “actively replicating infectious virus that can spread to others” yet. “For me, what [reservoir] means is there are at least pieces of the virus, even if they’re not infectious, that are altering people’s immune responses after infection and potentially contributing to their symptoms,” he says.
Proal’s organization recently launched a series of studies using advanced imaging and tissue biopsies to better understand these reservoirs.
Proal believes the virus’s “genetic backbone” is creating viral proteins in the gut, lungs, and neurons, which eventually enter the bloodstream. Depending on its location, the reservoir may be replicating and generating proteins or inert.
“There’s all kinds of possibilities and nuances,” she explains. Does it persist more in certain body sites? Does it persist in one body site through a different mechanism?”
No conflict.
Long-term COVID study could be compatible with viral persistence ideas.
“These could all actually converge and come together in an interrelated way, so by no means are they necessarily mutually exclusive,” says Stanford University’s long COVID clinic co-director Dr. Linda Geng.
Viruses can damage the immune system in many ways. “A chronic reaction to something could lead to immune dysfunction and inflammation,” explains Abdel-Mohsen.
Palmer said that T cells produce cytokines, which “over long periods of time are not good for your body.”
Proal thinks viral reservoirs may cause microclotting and neurological symptoms via the vagus nerve, which travels throughout the body and sends inflammatory signals to the brain. “That can activate brain cells that drive neuroinflammation and cognitive issues.”
At the Wistar Institute, Abdel-Mohsen found that fungus from the lungs and intestines are leaking into the circulation of some long-term COVID patients.
“This can cause chronic inflammation” that alters immune cells to produce neurotoxic chemicals, he says. This “vicious cycle” may start with local inflammation and gut barrier degradation from gut virus reservoirs.
Abdel-Mohsen explains, “each one could be happening independently and leading to a problem, but they can also lead to each other.”
“There’s still a lot of questions,” adds Geng, who’s running a clinical research to see if a 15-day treatment of Paxlovid helps long-term COVID sufferers.
Expect results later this year. If it works, the drug eliminated an illness.
“There are still plenty of people who are suffering and we really need to be able to figure out answers for them,” Geng adds.
